|

Thyroid Science 5(6):CLS1-7, 2010

Fixed Dose Radioactive
Iodine Therapy in
Hyperthyroidism: Outcome and Factors Affecting it
in a Region in South India

Full
Text Free in pdf format

Ajit S.
Shinto, MBBS, DRM,DNB,PGDHA,
Leena Pachen, BSc, NMT,DNMT, and T.K. Sreekanth, BSc, MRT, DMRIT

Nuclear Medicine
Department,
Amala Institute of Medical
Sciences,
Amalanagar, Thrissur -555,
Kerala, India
Correspondence: Dr. Ajit
S Shinto, Nuclear Medicine
Dept.,
Amala Institute of Medical
Sciences, Amalanagar, Thrissur
-555, Kerala, India
Office Tel: 04872304163 Personal
cell: 09747714265 Fax:
04872304163
ajitshinto@gmail.com,
ajitshinto@yahoo.com
|
 Abstract.
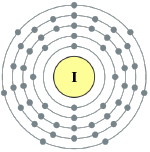
Objective: Radioactive
iodine-131 (RAI or 131I) has been
established as effective in the
treatment of patients with various
etiologies of hyperthyroidism.
However, the short-term and
long-term clinical outcome of
patients receiving RAI differs in
various studies. The aim of this
study was to assess the clinical
outcome one year after RAI therapy
and identify factors associated with
a good response.
Methods:
In this experimental study, 164
patients were included. They were
randomly selected from patients
referred to the Nuclear Medicine
Department for Graves’ disease,
multinodular goiter, or toxic
adenomas, which are indications for
RAI therapy. The radioiodine dose
was calculated based on the size of
the thyroid gland by physical
examination. Patients with normal
thyroid glands were administered
less than 10 mCi; patients with
large thyroid glands or thyroid
nodularity were administered a dose
of greater than 10 mCi
(approximately 15 mCi). Patients
were monitored closely clinically
and with blood investigations after
treatment for one year.
Results:
Among 158 patients who completed
follow up, 98.8% recovered and 1.2%
remained thyrotoxic. Among patients
who recovered, 74.2% became
hypothyroid and 22.6% euthyroid. The
incidence of hypothyroidism was 23%
in first trimester, 43.7% in second
trimester, 4.4% in third trimester,
and 3.1% in forth trimester.
Conclusion:
In our study, a good result was seen
in more patients than in other
studies. The better outcome may be
related to higher absorption of
radioactive iodine in our region.
The highest incidence of
hypothyroidism was in the second
trimester, so we recommend that
patients should be carefully
followed in this posttreatment
period. Abstract.
Objective: Radioactive
iodine-131 (RAI or 131I) has been
established as effective in the
treatment of patients with various
etiologies of hyperthyroidism.
However, the short-term and
long-term clinical outcome of
patients receiving RAI differs in
various studies. The aim of this
study was to assess the clinical
outcome one year after RAI therapy
and identify factors associated with
a good response.
Methods:
In this experimental study, 164
patients were included. They were
randomly selected from patients
referred to the Nuclear Medicine
Department for Graves’ disease,
multinodular goiter, or toxic
adenomas, which are indications for
RAI therapy. The radioiodine dose
was calculated based on the size of
the thyroid gland by physical
examination. Patients with normal
thyroid glands were administered
less than 10 mCi; patients with
large thyroid glands or thyroid
nodularity were administered a dose
of greater than 10 mCi
(approximately 15 mCi). Patients
were monitored closely clinically
and with blood investigations after
treatment for one year.
Results:
Among 158 patients who completed
follow up, 98.8% recovered and 1.2%
remained thyrotoxic. Among patients
who recovered, 74.2% became
hypothyroid and 22.6% euthyroid. The
incidence of hypothyroidism was 23%
in first trimester, 43.7% in second
trimester, 4.4% in third trimester,
and 3.1% in forth trimester.
Conclusion:
In our study, a good result was seen
in more patients than in other
studies. The better outcome may be
related to higher absorption of
radioactive iodine in our region.
The highest incidence of
hypothyroidism was in the second
trimester, so we recommend that
patients should be carefully
followed in this posttreatment
period.
Keywords
• Hyperthyroidism • Graves’ disease
• Radioiodine therapy • Outcome •
Hypothyroidism

Shinto, A.S., Pachen, L.,
Sreekanth, T.K.: Fixed Dose
Radioactive Iodine Therapy in
Hyperthyroidism: Outcome and Factors
Affecting it in a Region in South
India. Thyroid Science,
5(6):CLS1-7, 2010.
Full
Text Free in pdf format

© 2010
Thyroid Science |
|